Celtro Is Making Medical Implants Battery-Free Using Cadence Tools
The battery in a pacemaker occupies approximately 60 to 80% of its space, which limits the device’s placement within the heart. Celtro is looking to
In today’s medicine electronic devices are standard of care to interact with biological tissue, to measure and monitor biological signals and to substitute organ deficiencies. Cardiac device therapy is one of the oldest and most widely used clinical fields using implantable electronic devices.
Until today all medical electronic devices operate on batteries or external energy transfer. Autonomously driven energy self-sustaining medical electronics do not exist. Current technology of energy supply limits implantable electronic lifetime, it necessitates secondary replacement surgery with associated costs and risks, and it restricts functionalities of advanced biological signal monitoring to guide patient management and digital health.
Implantable cardiac electronics are further limited through typical out-of-organ implant sites which necessitate long insulated wires to connect to cardiac tissue. These so-called ‘leads’ carry a significant risk of insulation defect, wire break, infection and other vascular damage. With limited connection points to the target organ this technology contains further unmet risks of patient harm, repetitive surgeries and incremental healthcare costs.
Smart semiconductor implants for medical observation and actuation in the Nano-Watt range.
Energy harvesting and electrical stimulus directly interfacing with the cells.
Biological cells provide the energy for the function.
Wireless read and write interface to the device.
Based on a number of European-Patent-Office- and PCT-filings, we hold a strong IP position on technology, which allows to collect electrical energy of living biological cells with the purpose to sense, communicate and process electronic actions in medical electronic devices such as loop recorders and cardiac pacemakers.
Our basic operating principle enables collection of electrical energy in the Nano-Watt range. Its provenience is located in the action potential cycle of the living cell, which transforms sugar as primary energy carrier into electrical current flow as well as nerve and muscle action. We also employ system redundancy and time-domain differences between semiconductors and biology for increased efficiency. Our technology allows for storage, transformation and usage of Nano-Watt-Power to supply the energy needed to operate medical electronic components.
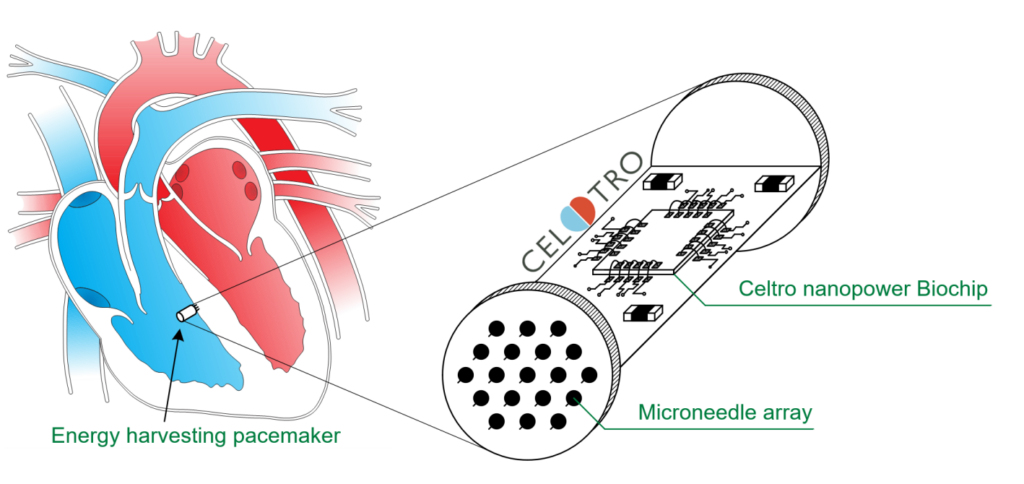
Application Pacemaker Cardiac pacemaker therapy is one of the oldest clinical electronic applications. During every single heartbeat, billions of cardiac cell are orchestrated in their synchronized function through a wave-like spread and magnification of electrical activation. Our technology utilizes this biological characteristic for multi-point electrical energy harvesting in substitution of deficiencies in electric organ functionalities, if they occur (see graphic).
Our first implantable product will be a pacemaker, which contains a semiconductor chip, operateting in the Nano-Watt-Range. Numerous electrodes connect the chip with the cardiac tissue. The device will operate without leads and without batteries. The electrodes to the biological tissue will provide a high number of mutually replaceable connection points to the tissue, leading to higher reliability of the entire device-to-tissue interface. The product will become smaller in volume and removes the need for replacement when batteries are depleted.

Gerd Teepe, PhD

Jarek Budny, MBA

Paul Reidy, Esq

Forrest Pape, MSEE

Thomas Gaspar, MD

Judith Piorkowski, MD

Mike Pederson, MBA

Prof. Dr. Kai Simons

We are hiring miroelectronic engineers. You are interested to join our team? Please write an e-mail to gerd.teepe@celtro.de.
„CELTRO was founded on November 18th, 2019. Its initial work has focused on feasibility studies, system architecture, creation of the development-partner-network and own patent filings. We are now expanding operationally to develop the prototypes leading into qualified products.“
Backed by venture capital from private investors.

The battery in a pacemaker occupies approximately 60 to 80% of its space, which limits the device’s placement within the heart. Celtro is looking to
Bioelectric energy harvesting from myocardial tissue is feasible and will be able to supply the energy to operate autonomous miniaturized pacemakers in the future. CELTRO
Heart Rhythm Society – Annual Conference from April 24-27 in San Diego, USAForrest Pape is presenting the Celtro-Concept for an autonomous pacemaker without batteries, as
Celtro presented at the Industry Strategy Symposium, which took place from 13th to 15th of March 2025 in Sopot, Poland. The conference is organized by
Celtro’s partner for package manufacturing, Nano Dimension, has shared a customer success story video on Celtro’s innovative biological energy harvesting technology.
The online journal Wired recentlly published an article on Celtro and its energy harvesting technology: https://www.wired.co.uk/article/the-battery-that-never-gets-flat
© Celtro GmbH, 2021-2024